- Refer a Patient
- Referral Types
- Patient Information
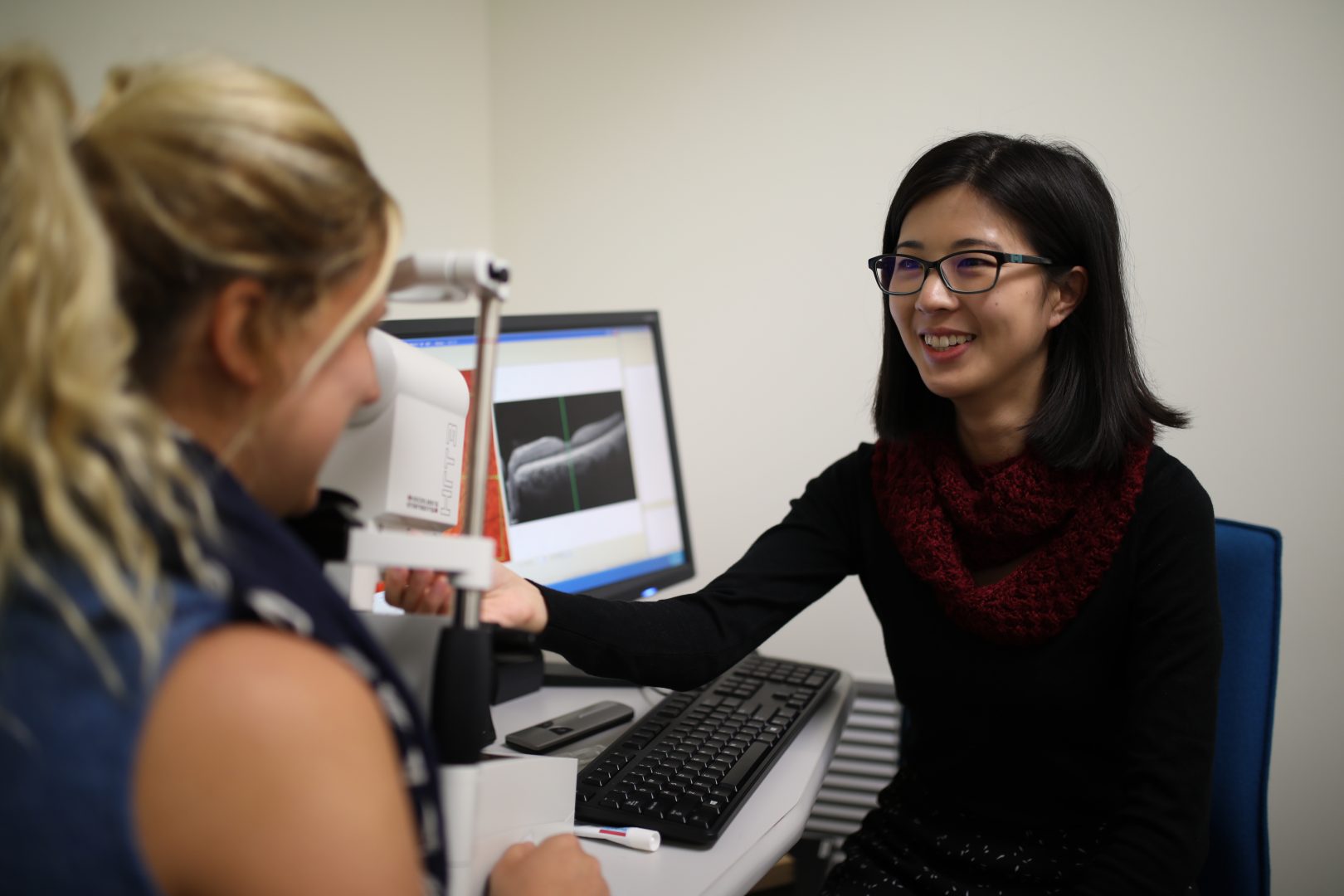
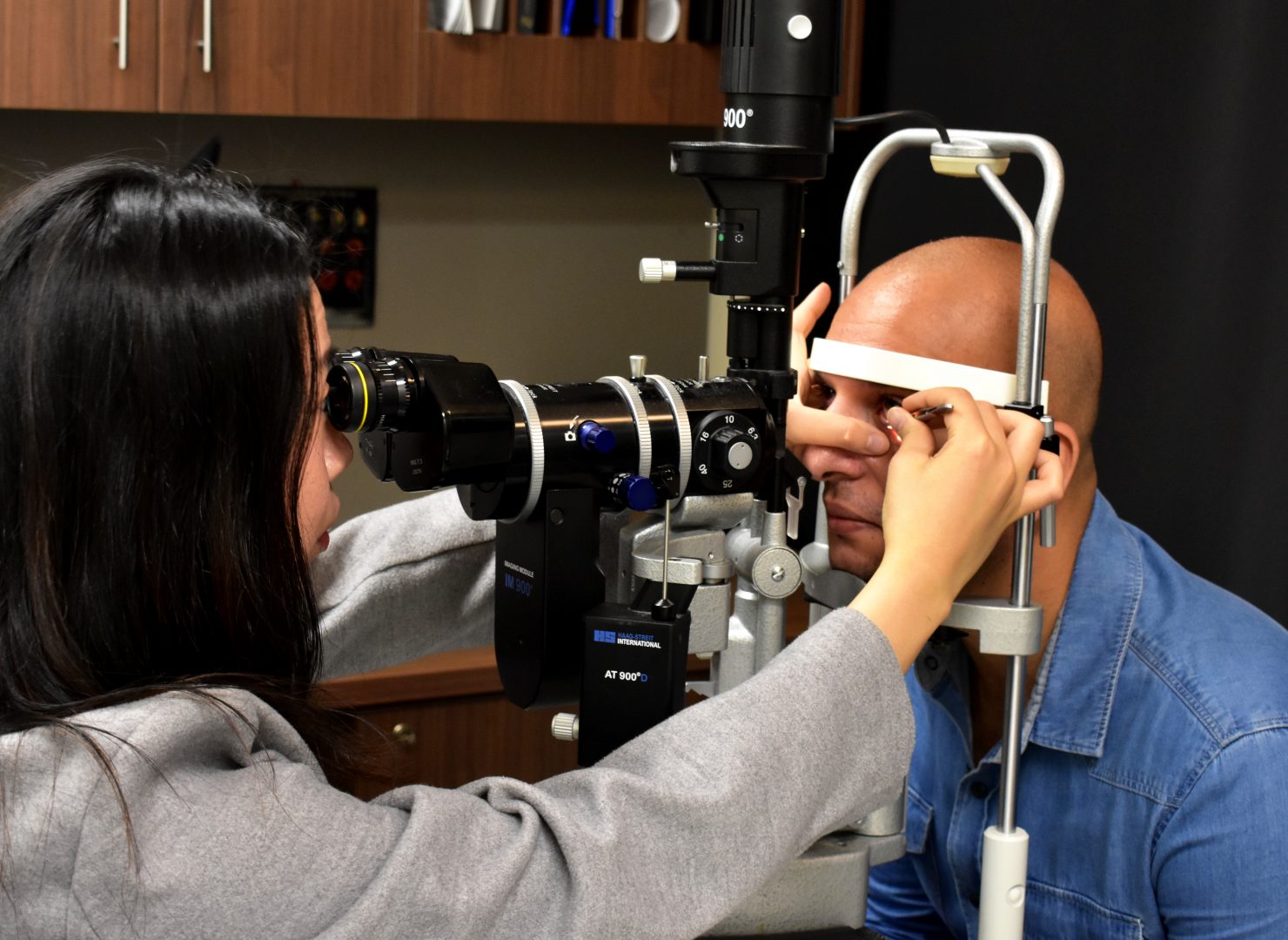
- Overview of CFEH Clinics
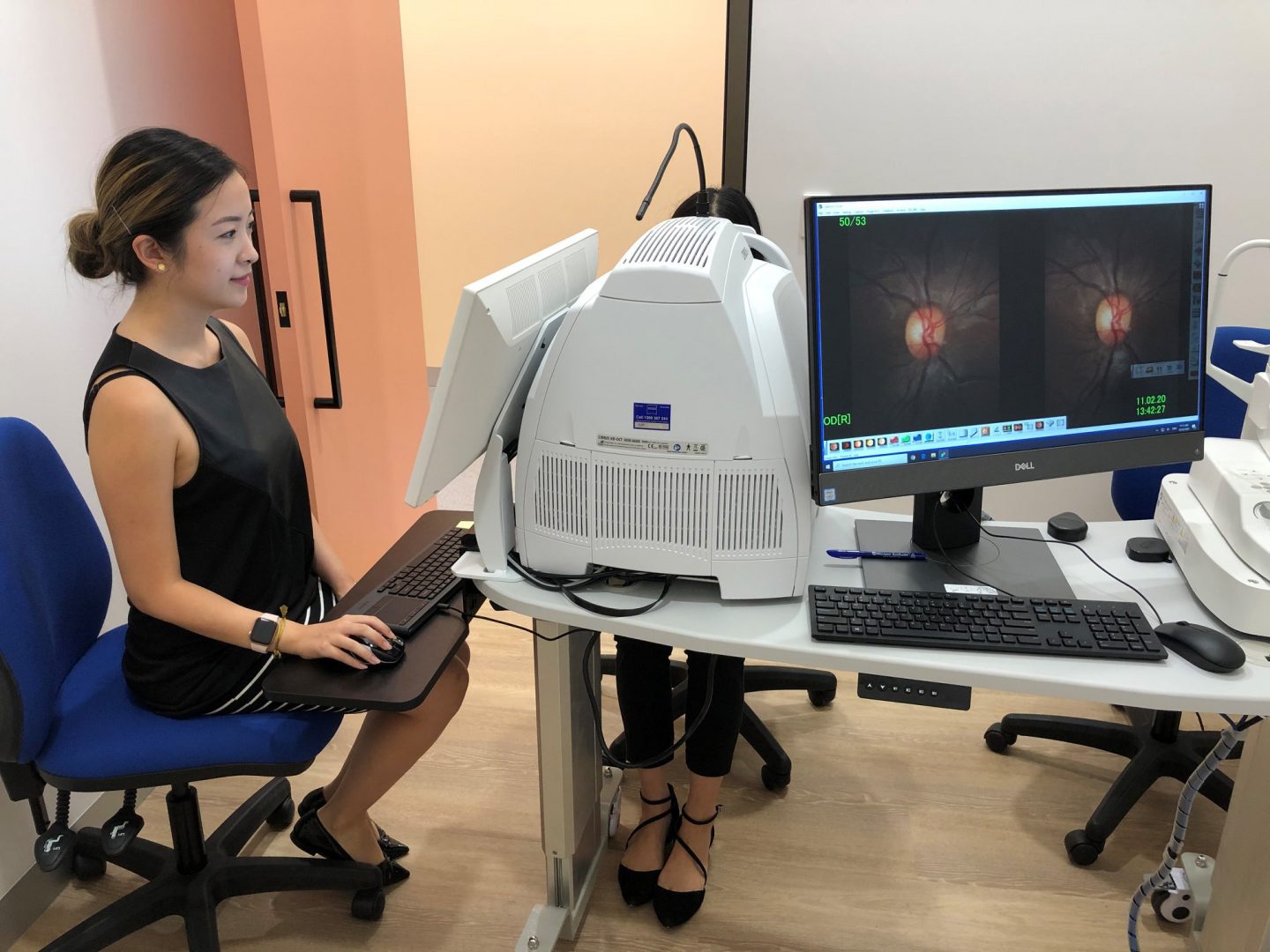
- CFEH Instrument List
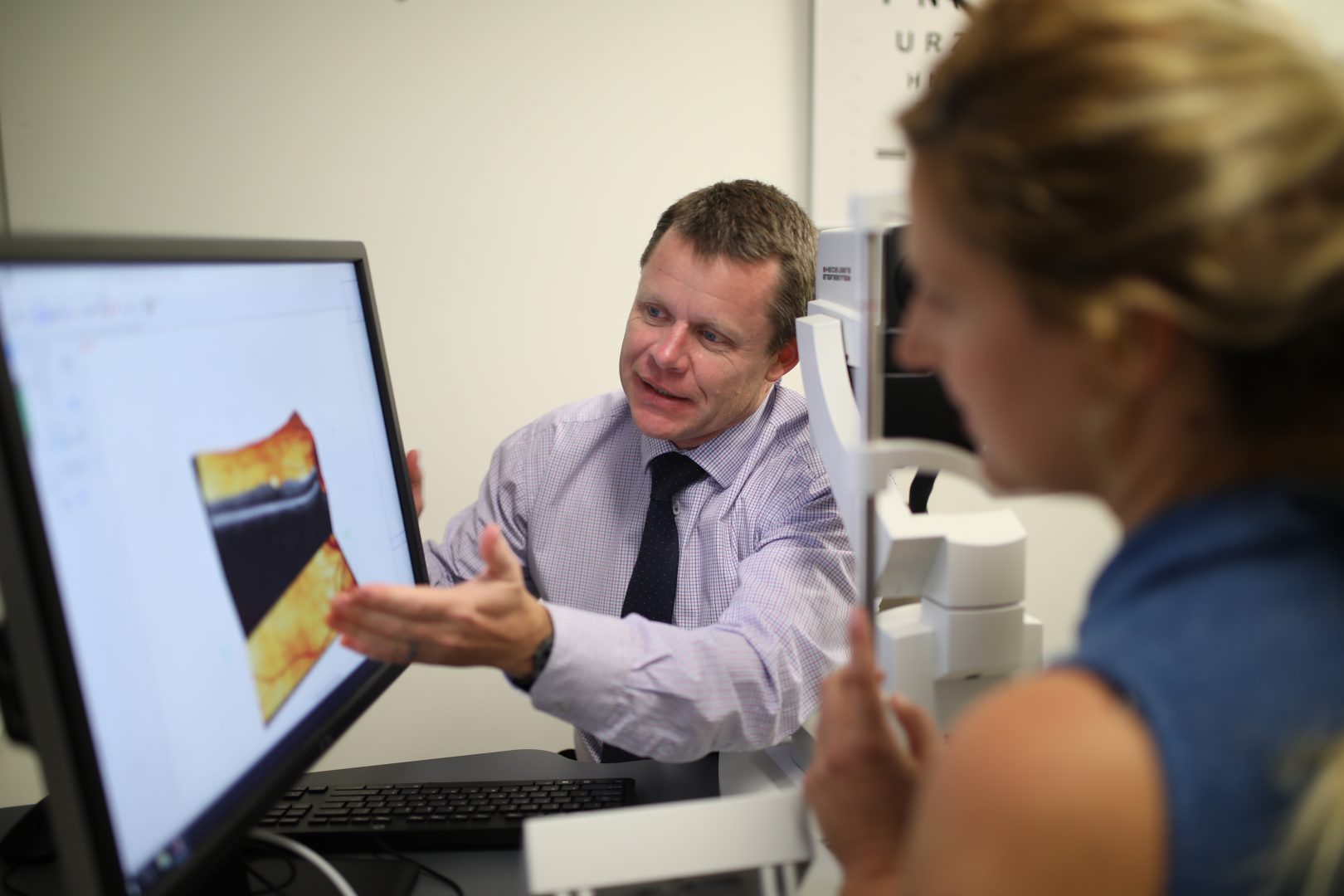
- Our clinical team
- Causes of Vision Loss
- Patient Forms





An Extract from the CFEH Atlas
Congenital Stationary Nightblindness
Overview
Congenital stationary night blindness (CSNB) refers to a group of conditions that have an abnormal dark adaptation curve, abnormal electroretinogram and symptoms of difficulty with night vision. Visual acuity is typically in the range of 6/9 (20/30) to 6/60 (20/200) and the condition is often associated with myopia of varying degrees.
Nystagmus and strabismus are often also associated with this condition. Colour vision is typically normal and in most forms of CSNB fundus examination is also normal. The two exceptions to this are Oguchi disease and fundus albipunctatus which will be outlined below.
Electrophysiology testing in CSNB typically shows a reduced scotopic b-wave amplitude to a flash stimulus after dark adaptation. An electronegative wave results whereby the amplitude of the a-wave is greater than that of the b-wave.
The name of this group of conditions is a misnomer in that they are not truly “stationary” – some worsen over time leading to reduced visual acuity or constricted fields with age.
Oguchi Disease
Oguchi disease is a form of congenital stationary night blindness associated with a golden coloured fundus that changes to a normal colour after prolonged dark adaptation (the Mizuo-Nakamura phenomenon).
Patients with oguchi disease also have unusual results on dark adaptation electrophysiology testing. These patients take 1-2 hours of dark adaptation before rod sensitivity recovers and they can see in a dimly lit environment. After prolonged dark adaptation, a single flash of light will elicit a normal a and b wave. There is no response however to a second light flash until another period of dark adaptation has been completed.
Fundus Albipunctatus
Fundus albipunctatus is a form of congenital stationary night blindness that is characterised by numerous small, white-yellowish retinal lesions throughout the retina, sparing the fovea. It shows an autosomal recessive inheritance pattern and is associated with mutations in the RDH5 gene.
A patient with fundus albipunctatus will have normal fields and acuity unless tested with a dim stimulus which will cause both a reduction in acuity and constriction of visual field.
Although rod function has not been shown to significantly reduce over time, there is a high incidence of associated cone dystrophy with this condition with age (over 30%). The development of a concurrent cone dystrophy will affect colour vision, visual acuity and central visual fields.
- Case 1: Fundus Albipunctatus
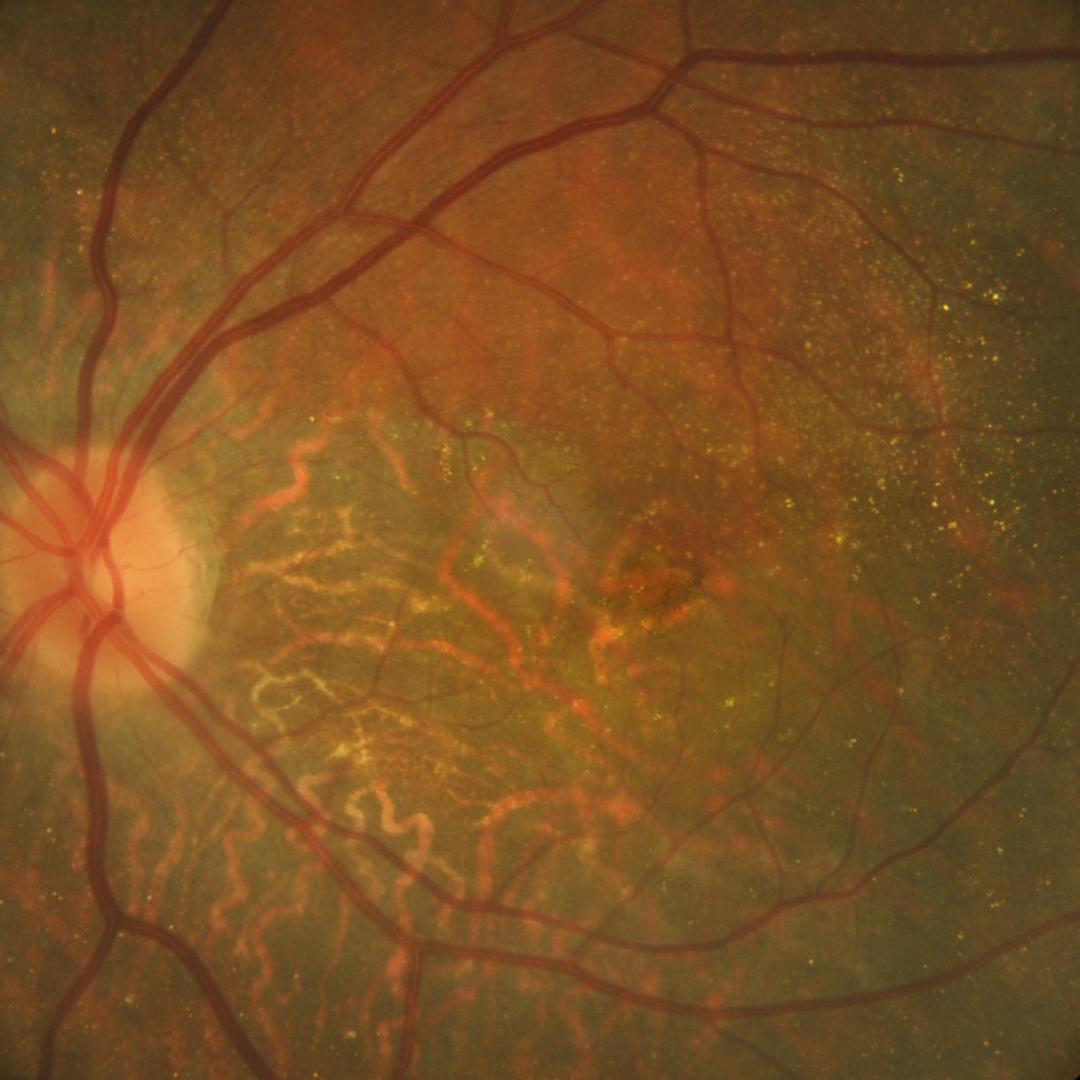
A 51-year-old Caucasian female with difficulty seeing in the dark and in bright sunlight. She has noticed problems for 5 years but feels they are getting worse. She has been diagnosed with fundus albipunctatus and cone dystrophy by an ophthalmologist – a diagnosis confirmed with electrophysiology testing.
Her best-corrected visual acuities are 6/6+ (20/20+) in the right eye and 6/4.5- (20/15-) in the left.
Colour vision testing with the L’Anthony de-saturated D-15 was failed with 6 crossings in the right eye and 3 in the left.
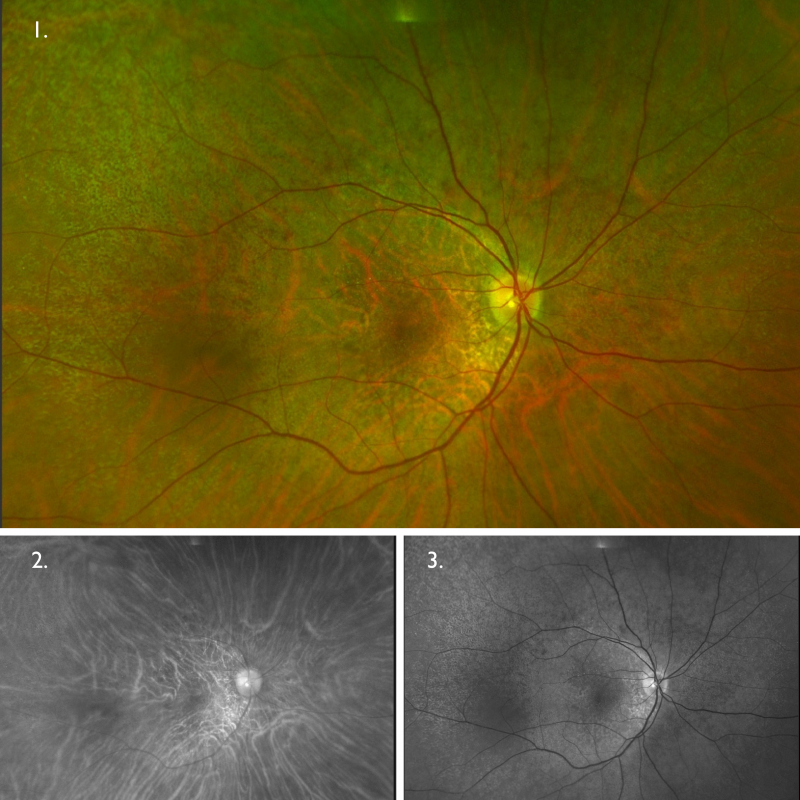
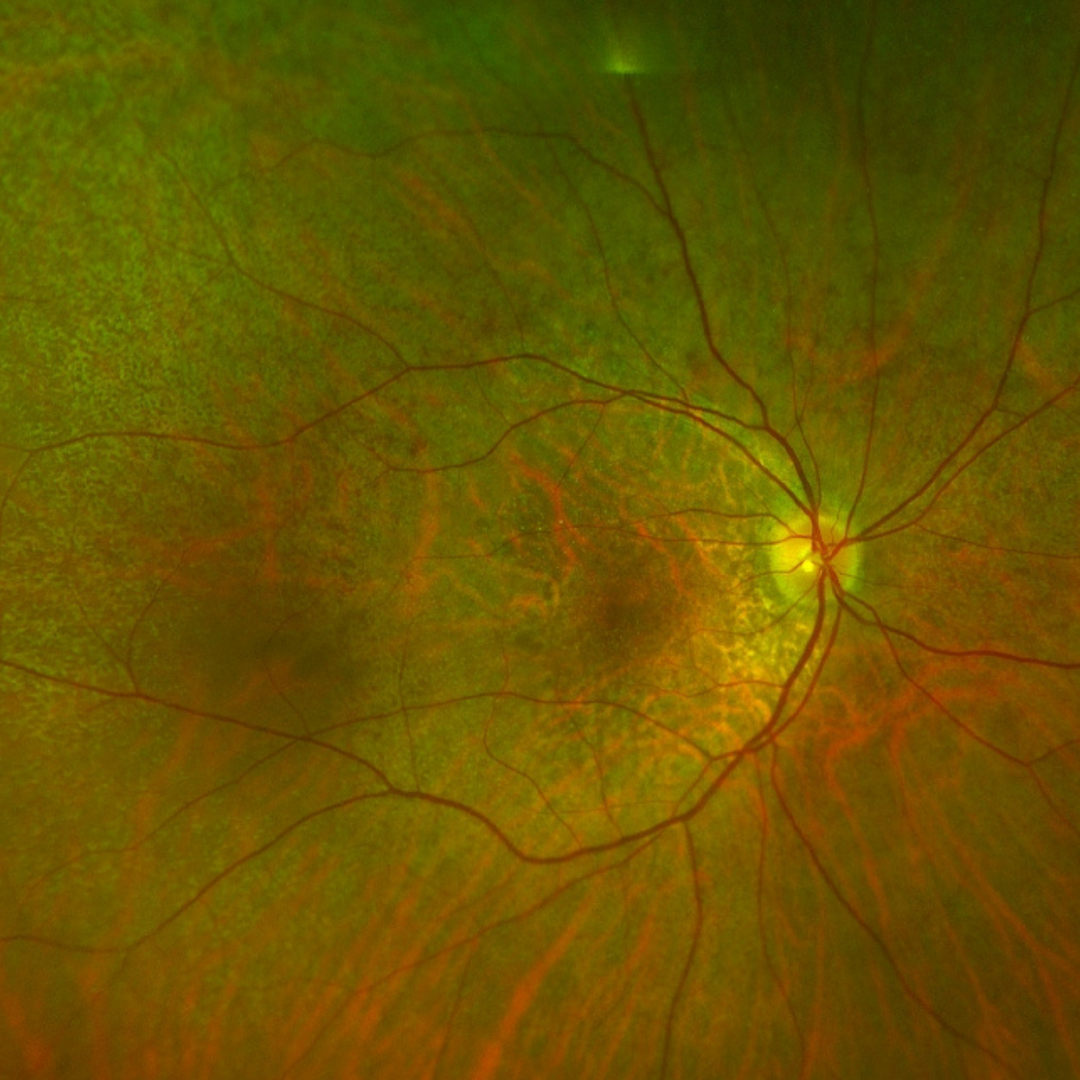
Optomap (1), red separation (2) and green separation (3) images – right eye: Widefield imaging shows small pale lesions scattered throughout the fundus with a relative sparing of the macula.
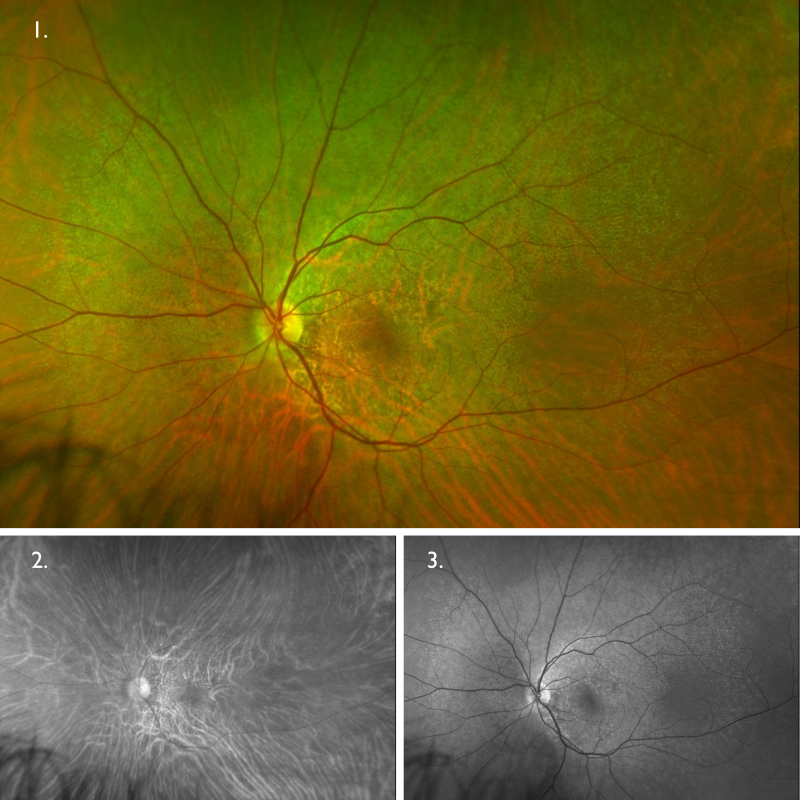
Optomap (1), red separation (2) and green separation (3) images – left eye: Widefield imaging shows small pale lesions scattered throughout the fundus with a relative sparing of the macula.
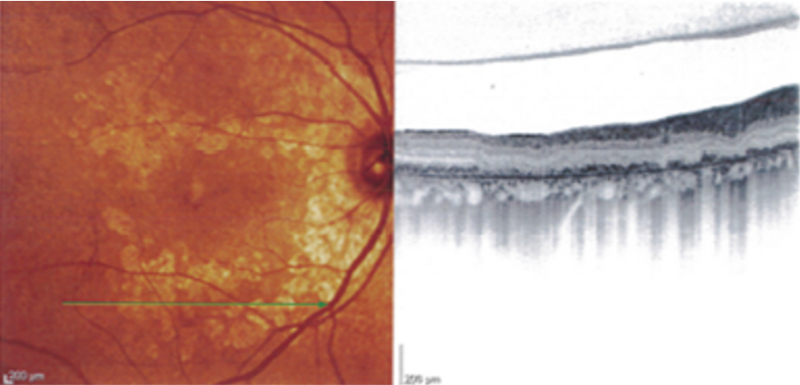
Spectralis OCT line scan through the pale lesions shows outer retinal atrophy.
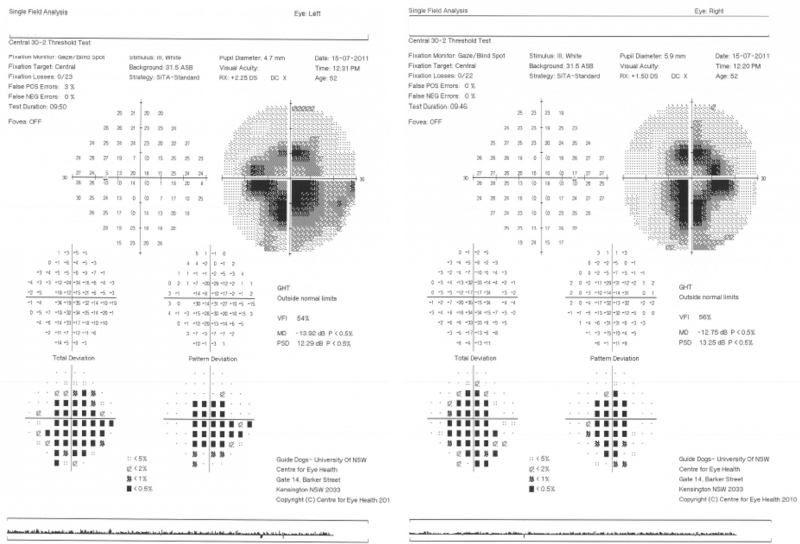
30-2 fields show central and paracentral visual field loss (but more inferiorly) in each eye.
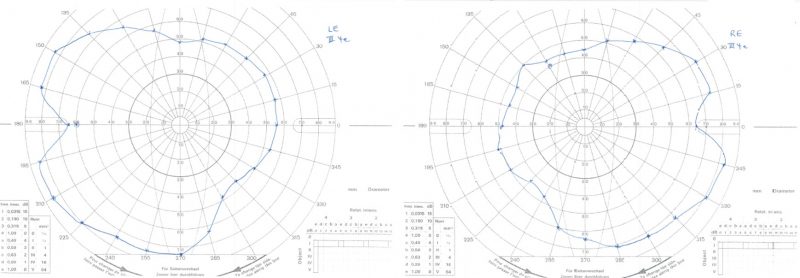
Goldmann kinetic perimetry showed the extent of the visual field to be approximately in the right eye: 65º temporally, 50º nasally, 45º superiorly and 65º inferiorly, and in the left eye: 65º temporally, 55º nasally, 50º superiorly and 75º inferiorly with the III4e stimulus. The right inferior extent and the nasal and superior extent in each eye were slightly reduced compared to normal values.
Differential Diagnosis
Other differentials to consider is retinitis puctata albescens (more information on this condition may be found in the CFEH Atlas).
References
MacDonald IM, Hoang S, Tuupanen S. X-Linked Congenital Stationary Night Blindness. 2008 Jan 16 [Updated 2019 Jul 3].
Nakamura, M., Hotta, Y., Tanikawa, A., Terasaki, H., Miyake, Y. (2000) A High Association with Cone Dystrophy in Fundus Albipunctatus Caused by Mutations of the RDH5 Gene. Invest. Ophthalmol. Vis. Sci. 41(12):3925-3932.
Skorczyk-Werner, A., Pawłowski, P., Michalczuk, M., Warowicka, A., Wawrocka, A., Wicher, K., Bakunowicz-Łazarczyk, A., & Krawczyński, M. R. (2015). Fundus albipunctatus: review of the literature and report of a novel RDH5 gene mutation affecting the invariant tyrosine (p.Tyr175Phe). Journal of applied genetics, 56(3), 317–327.
Thaddeus P Dryja (2000) Molecular genetics of Oguchi disease, fundus albipunctatus, and other forms of stationary night blindness: LVII Edward Jackson Memorial Lecture, American Journal of Ophthalmology, Volume 130, Issue 5, Pages 547-563.